An African health minister’s dilemmas
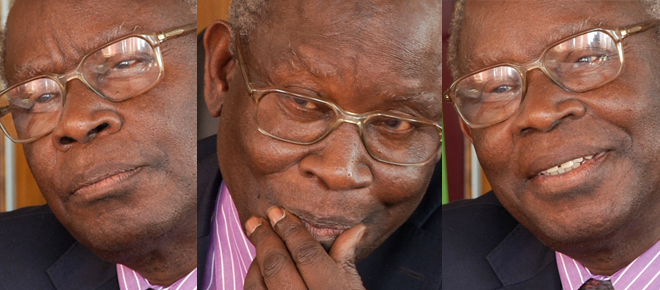
The Cola Road, Week 3: Claire Ward in conversation with Dr. Joseph Kasonde
Share
Claire Ward is a former associate editor at Maclean’s and is pursuing a Master’s in news and documentary at New York University. She is blogging from Zambia, where she is filming The Cola Road, a documentary that follows the launch of the first aid program that aims to use Coca-Cola’s distribution network to deliver medicines to the remotest corners of the developing world. Check out more updates from The Cola Road on Facebook at: www.facebook.com/TheColaRoad or Twitter at: www.twitter.com/TheColaRoad. Or follow Claire on Twitter @thementalward
Last week, I sat down with Zambia’s minister of health, Dr. Joseph Kasonde. At his offices in Lusaka, we discussed aid, the benefits and perils of public-private partnerships, and specifically U.K. charity ColaLife’s idea of teaming up with Coca-Cola to distribute medicines to rural areas in this country. He had lots to say:*
Q: Can you talk about the challenges of access to medicine in Zambia?
A: What happens is the medicines are delivered to a place some 200 kilometres away, and you have to find a way to get them from there to the village to the people who live around it. When you send a lorry from the centres like Lusaka and Ndola, they can only so often. They can’t do this on a very regular basis. And if you want deliveries weekly or daily then you’ve got to do something local. And that is where the private sector comes in. They have shown, as ColaLife has taken up, that you will find Coca-Cola in any village, at any time, in the course of the year. But you’ll not find medicines. What’s the difference? There is something there to learn from. And that’s what we’ve done.
Q: What potential do you see for ColaLife? Do you think the idea of delivering anti-diarrhea kits containing oral rehydration salts through Coca-Cola’s distribution network is sustainable?
A: It’s a very interesting project which we support as a ministry, because the whole idea of distributing these important salts has been lacking for a long time. (…) I’m trying to build on their concept for the delivery of medicines in general, as it applies particularly to the rural areas.
Q: Do you mean to borrow the public-private-partnership model?
A: I’m following from the PPP concept, as applied by ColaLife; namely where you define what is to be delivered, you identify who at a certain locus is capable of delivering, and discover how many people who want to do this and then take them into account in your planning.
Q: Can you tell me more about how it’s going to work in practice?
A: We are talking of starting very soon to adopt this concept for the supply of medicines at the last mile. That means we identify a suitable retailer in a village or small community, we agree with them what it would cost if they were to bring the drugs to a place 50 or 100 kilometres away, we pay them, they bring that material to the nearest health post or health centre.
Q: Why can’t the public sector reach the last mile by itself?
A: Medical Stores Limited [the parastatal organization that delivers medicines for the Ministry of Health] has been grappling with this problem for some time. I think they now have got some ideas for how best to deliver at that level. And so this idea came in as a real bonus, because they had been thinking along those lines but not quite grasped the use of the local entrepreneur for the purpose. So this is what they’re now going to develop further and use.
Q: Is the association with Coca-Cola a concern?
A: I was in the happy position where most of the negotiations between ColaLife and the ministry had already been done, and I just came in at a point where they needed to sign that memorandum. So I saved myself from sweating about Coca-Cola and cigarettes and any of the bad things that they could do potentially, and concentrated on the good things that we could do. I’m afraid I must escape that issue and go straight to the good things.
Q: But how do you feel about the positive benefit to Coca-Cola?
A: Well, there were worse options. They could have chosen beer, for example, and gone around the country and said ‘but you can get your beer here, why don’t you get your medicines?’ So I think the principle is so good, it can even do harm. That’s the kind of situation we are in. But it’s going to do good.
Q: Had the thought of partnering with Coke ever occurred to you before?
A: No. You have to look at it in the historical context of relations between public sector and private sector as life has developed in developing countries. There was a period of suspicion between the two, and any thought that these money-seeking characters could actually do good was not acceptable at that time. As we have grown over the generations we have come to accept capitalism as having potential benign effects as well. So [in the past] the atmosphere was not conducive. What our government has done is make clear that we accept the role of the private sector and the collaboration between public and private. So in that sense we have provided an enabling environment for doing that.
Q: What about the role of aid organizations in Zambia? Where do you think aid fits in Zambia’s future?
A: We have not had a problem with accepting aid. We have talked more in terms of partnerships. Sometimes the old version of donors coming and giving with their own agendas has come to the fore, but it’s not our thinking at present. Our thinking is, you have a partner, you have a common objective, and their participation may be in the form of a donation, but your participation is in the form of defining the needs and sharing with them the reasons why. And so we are talking of partners, not of donors, and we are quite comfortable.
Q: How did you react to ColaLife’s approach within Zambia?
A: What they are saying is that they have a concept, they have a workable idea, and they feel nevertheless that government should be aware and accept what they are proposing, which we have done. So I think it shows that even on the part of the so-called donors, there is new thinking. (…) They feel they want to be part of our decision-making in adopting a new technology or process, and not to tell us ‘this is the way to do it, this is the way we’ve always done it in Europe, now you do it this way and you will succeed.’ So I think there has been a lot of technical competence in ColaLife and I think a lot of political sensitivity as well. And cultural sensitivity. These sensitivities cannot be ignored. And it’s good that they have grasped that.
Q: Have you gone out and visited rural health centres and met families?
A: I have been out many times, in fact I’m more times out than in. Apart from that, I was myself, as a child, bred in a rural village. So it’s not new to me. But I have to keep acquainting myself with the current version of living in a rural area. So I have been out in many places across the country. (…) I think in many countries you find people drifting to the urban areas because of what is there. But I think there is also a feeling now that you can do something at home in your village, if you wish to stay in your village. I’m finding that an encouraging message.
Q: I’ve heard that witchcraft and superstition are still alive and well in some rural villages. Is there an issue of people rejecting modern medicine?
A: Yes, (…) there are many who believe the potential of traditional healers or maybe herbalists or diviners and what they can do. So we live with that. (…) We do not say ‘don’t listen to those cultural beliefs, don’t go to those traditional healers.’ No, (…) we offer an alternative. We say, ‘there is this modern alternative,’ we make it available, and gradually most people get to buy into that. But we will not stop them from following any beliefs they have, unless it becomes a risk to their lives, in which case we are talking of crime.
Q: What is on Zambia’s horizon in terms of public health?
A: I think you have to look at it from the point of view of our phase in development. We were at a previous phase — when we had 125 health centres in the country — where the critical issue was just to create buildings to operate in. Then the critical issue of when we didn’t have university graduates at all, we had to think of creating universities and training university graduates. We were in the phase of quantity. I like to believe we are now in the phase of quality (…) So our principles at this stage in our development are very clear: One, universal access to whatever services we are providing; two, improvement in the quality. (…) After that there will be other phases, but I’ve got enough on my plate with this phase, thank you.
*This interview has been edited for form and brevity by Maclean’s.