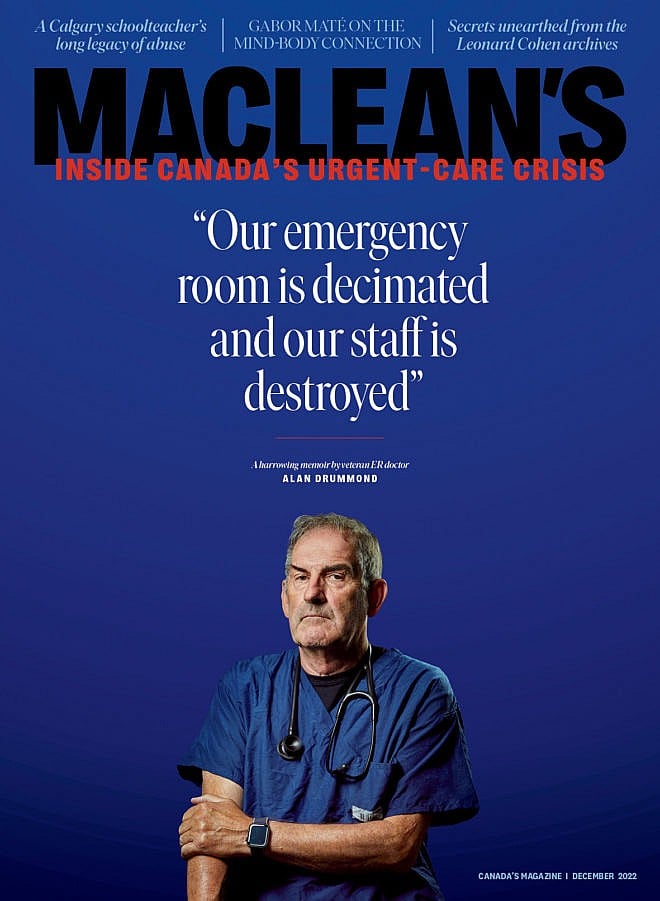
State of Emergency: Inside Canada’s ER Crisis
I’ve been an urgent-care doctor for 39 years, and my department has never been closer to collapse. We’re not alone.
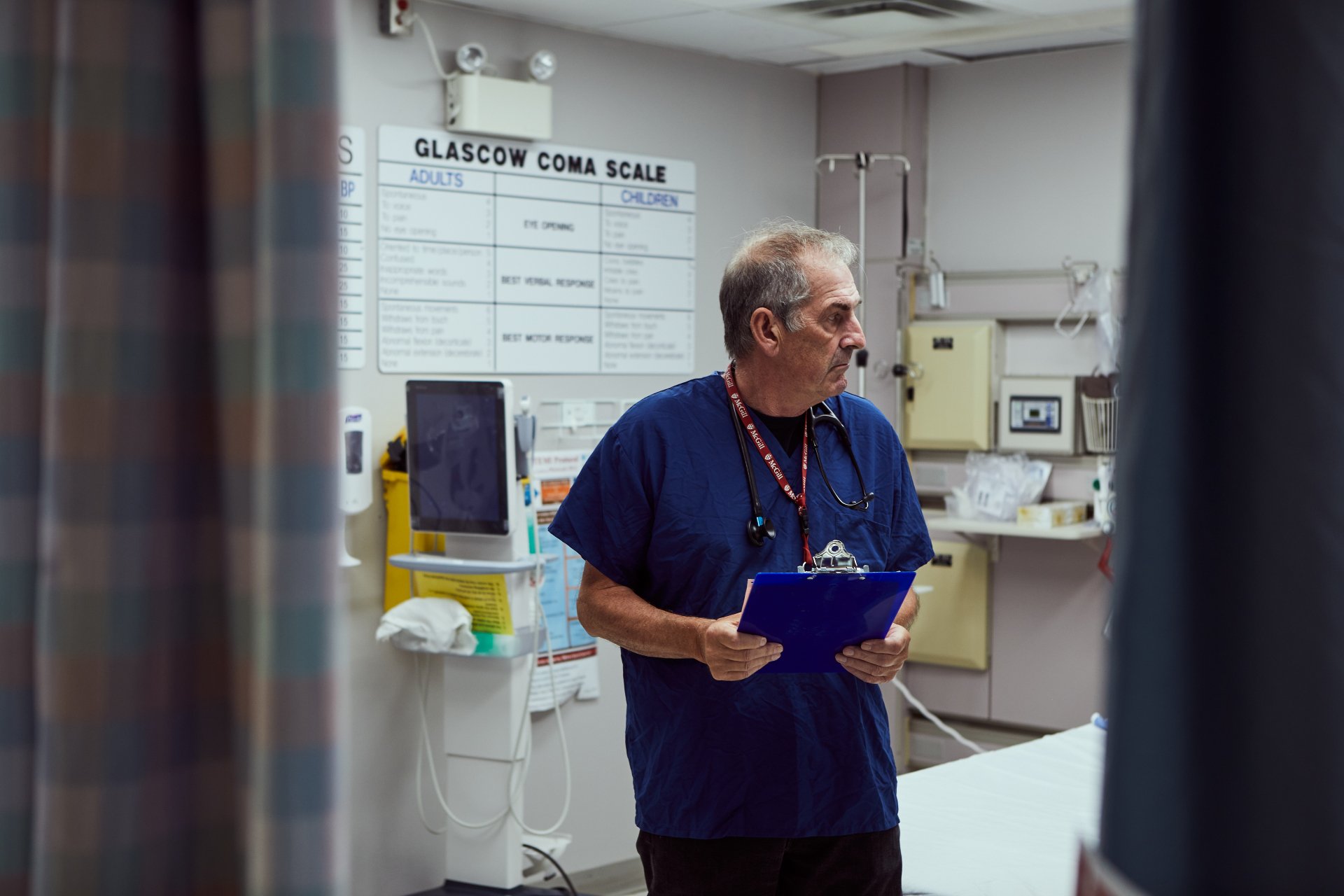
(Portraits by Rodolphe Beaulieu)
Share
A few months ago, a middle-aged woman in seemingly fine health came to my ER, feeling under the weather. She had called her family doctor, but he was booked up and couldn’t see her for six weeks. I treated her instead, and when I pulled up her records, I saw a recent scan ordered by that same doctor, the results of which she hadn’t yet learned: cancer, already too advanced to cure. It wasn’t just one tumour; they were everywhere. It was up to me to tell her she had a handful of months, at most, and she should start getting her affairs in order.
There was nothing else to do but hold her as she cried. She asked me what would happen to her spouse—who is older than her and dependent on her—when she was gone. More than anything, I wanted to say I could get her another year, or two or five. Instead, she heard the hardest news of her life from a stranger wearing a mask and a shield, in an exam room steps from the noise of gridlocked hallways and a packed waiting room.
For 39 years, I’ve worked as an ER physician at Great War Memorial hospital in Perth, Ontario, part of the Perth and Smiths Falls District Hospital. After all that time, I’ve become intimately acquainted with life’s fragility—how any of us can be here one moment and gone the next. That’s part of the job. But medicine shouldn’t be so ugly and upfront and harsh. Patients shouldn’t have this kind of news delivered in an overcrowded, underfunded emergency department by a person they’ve never met. More and more often, however, these heartbreaking, infuriating scenes are playing out in my hospital and in countless others across the country. Why? In part because the pandemic delayed checkups and put routine scans on the backburner. More patients discovered how sick they were, or that they were sick at all, during visits to ERs that were already struggling and in no condition to substitute for day-to-day health-care providers.
Yet we can’t simply blame this crisis on COVID—that’s the easy way out. Canadian health care, both primary and emergency, has been buckling for decades, and I’ve had a front-row seat to its slow collapse. For the past 21 years, I’ve been public affairs co-chair of the Canadian Association of Emergency Physicians, the professional association for Canada’s emergency doctors. I’ve always seen our emergency department in Perth as a microcosm of Canada. Everything that happens here is also happening in the roughly 850 emergency departments nationwide: overcrowding, staff shortages, violence, abuse, burnout, patients warehoused in the ER because they can’t get a bed. What happens in Perth happens everywhere, and what’s happening in Perth has never been as bad as it is today.
Wait times for non-admitted patients to see a doctor have shot from one hour to five. Patients who need a bed might wait 24 hours or more (the provincial average for emergency patients is 21 hours). Sometimes it’s even longer: early in October, I came in for a shift to find five patients waiting for admission. When I came back the next day, they were all still there. Admissions take longer, which means treatment takes longer, which leads to more complications and higher mortality.
Under these conditions, it can be nearly impossible to maintain the compassion and care that should be intrinsic to our profession—the humanity and decency that good doctors bring to their work. A humane ER is not one in which patients are dying in the halls, as we’ve seen in Canada these past two years. It’s not one where seemingly healthy people learn of terminal diagnoses in exam rooms commandeered for brief moments of privacy, or where violence and abuse have become run-of-the-mill.
Our lowest point in Perth—so far—came in July, when our ER shut down for nearly four weeks. The closure left a town of 6,500 people, and the tourists who flock here in the summer, with only bare-bones access to emergency services. Our closure was unprecedented in its length and severity, but predictable in hindsight. In province after province, reduced hours and shutdowns have become distressingly common. And while the pandemic accelerated the decline, the rot was evident decades ago, in the form of neglect, under-investment and the devaluing of the doctors and nurses who keep our emergency departments running day to day. The decline of the primary-care system has only put more strain on us. For those paying attention, the origins of today’s crisis were visible years ago—even in a little ER like mine.

***
I’ve always loved emergency medicine. There’s a wild, satisfying, anarchic breadth to the work. Since 1983, I’ve been a family physician in Perth, serving around 1,500 patients, and I’ve worked as a coroner as well. But emergency is my true passion—I’m hooked on the anticipation and adrenalin, on never knowing what will come rolling through the door. In the ER, you have to master the art of turning chaos into calm, of moving from the tragic to the mundane in the blink of an eye. You may need to leave the weeping family of a cardiac-arrest victim to attend to someone with back pain, or go from a man with terminal liver disease to a guy calling you a “COVID Nazi.” You need to appreciate the good and the bad in humanity and maintain a sense of humour (preferably a dark one) about it all. Rural emergency medicine requires even deeper commitment. Small-town physicians live where we work—our patients are often our neighbours, and we’re personally invested in our hospitals.
With 49 beds, Great War Memorial is small but mighty, covering a vast rural area and treating 25,000 emergency patients each year. When I got to Perth as a young doctor, after internships and residencies in Montreal, Ottawa and Vancouver, emergency medicine in Canada was barely considered a specialty. Instead, it was something of a dumping ground for old surgeons, or new immigrants who faced barriers to setting up practices. This lack of interest in emerg was especially prevalent in rural hospitals. By the late 1970s and early ’80s, it was becoming clear that it would be beneficial to have physicians who specialized in cardiac and other trauma emergencies. The focus became on educating and training staff to identify and treat life- and limb-threatening crises.
That’s what we did in Perth, where I made it my life’s work to transform our emergency department. In 1988, I became the department’s medical director, a job I held until 2012. I started by bringing in trauma surgeons and emergency doctors from Ottawa and Kingston to tell us what happened to patients we’d sent to hospitals there, and to help us break down to the minute what we could have done differently with them. Our doctors and nurses took emergency certification courses, and we set up study programs and performance reviews. We did away with onerous 24-hour shifts to make sure doctors and nurses were well rested rather than exhausted and crabby. We committed, in tangible ways, to transforming the department for the sake of our patients.
I worried our staff would get sick of it and quit; for a small-town ER, this kind of levelling up was unusual. But it paid off. In 2013, CBC’s The Fifth Estate did a special report on Canadian hospitals and gave ours an A+ rating. I was incredibly proud to know that our hard work was being recognized. Patients knew that when they got here, they’d be treated by people who truly cared.
In ERs from St. John’s to Victoria to Iqaluit, life-threatening emergencies requiring immediate attention make up only a tiny part of the patient load, maybe two per cent. Other patients, who need to be seen within an hour—heart attacks, pneumonia, appendicitis—represent another 20 per cent or so. Then there’s everything else: vague pains, broken bones, wasp stings. One major difference between a rural ER and an urban one is that we see more cases that would otherwise go to a walk-in clinic. Part of our mission is to be there as a stopgap. In recent years, though, that stopgap has been stretched far beyond reasonable limits.
There wasn’t a single free bed, but patients kept coming. On days like that, there’s no privacy, no confidentiality, no dignity.
The number-one issue today in Perth, as in most ERs in Canada, is overcrowding, and all the knock-on effects that follow from it. Overcrowding—loosely defined as being unable to care for patients within a maximum of four hours—was first identified as a problem in Ontario in the late 1980s. It became so severe in Toronto that in the 1990s, the Ontario Hospital Association launched a task force to tackle it. One major problem identified was a lack of beds. In the last half of the ’90s, the number of acute-care beds in the province fell by 22 per cent, even as demand rose thanks to a growing and aging population. In 1995, the occupancy rate for those beds was 85.6 per cent. That’s not bad—a safe hospital is defined as one with 85 per cent occupancy or less. By 2000 it had climbed to 96 per cent. Some hospitals in Canada now exceed 100 per cent, with patients spilling into any hallway or exam room or other corner that can accommodate them. One Wednesday evening this past July, the Lanaudière Hospital in Saint-Charles-Borromée, Quebec, peaked at 191 per cent capacity. In 2021, the Organisation for Economic Co-operation and Development ranked Canada 31st among 34 countries for acute-care capacity, with 1.97 beds per 1,000 people. (Japan, at the top of the list, had 7.74.)
We can see the effects of this over-crowding every day. One afternoon this past summer, I came in for my shift and found every treatment stretcher occupied by admitted patients, with more in the OR recovery room. Because the recovery room was full, elective surgeries, for people who’d been waiting months for a knee or shoulder replacement, were cancelled. There wasn’t a single free bed in the building—and still people kept coming. The only place we could see patients was on chairs in the hallways. On days like that, there’s no safe space to assess a patient. There’s no privacy, no confidentiality, no dignity.
It’s no surprise our ERs have become full of tension, anger and violence, nor that ER staff have been on the receiving end of it, from raised fists and raised voices to streams of expletives to containers of bodily fluids tossed across the room. One patient’s irate husband stomped on, and broke, a doctor’s leg. Another patient reached for a cop’s gun. I once kicked someone out of the emergency department for yelling at a nurse, after I decided he didn’t need further attention. He later stalked my private office. Five years ago, a staff member at our sister site in Smiths Falls was stabbed in the head with a pair of scissors. That same year, a nurse was nearly strangled at a hospital in Montreal.
The effect of all this is devastating on patients and staff alike. If you’re sitting in the waiting room with a sick child who has an ear infection, you don’t want a guy dropping F-bombs and making racist comments. If you’re lying on a stretcher in pain, it’s exhausting to also deal with somebody screaming beside you.
In 2015, health-care workers had more than twice the number of violence-related lost-time injuries that police and correctional officers had combined. And half of all attacks on health-care workers occur in emergency departments. Nurses, who spend the most time with the public, bear the brunt of it. That drives absenteeism among nurses higher and higher—nine per cent for full-time public-sector nurses in 2016, costing taxpayers an estimated $989 million.
In spite of it all, Canadians haven’t been deterred from visiting ERs. A 2016 analysis by the Canadian Institute for Health Information found that 41 per cent of the population had used an ER within the previous two years, more than citizens of other Western countries including the United States, France, the United Kingdom, Australia, Germany and Switzerland. Often this is because people can’t get appointments with their family doctor, or they don’t have one. And so the furious cycle continues.
***
COVID devastated our ERs. When it struck ours, we had 15 nurses working full time and part time hours in Perth. They were wonderful people who understood emerg, who were as addicted to it as I am. Nurses are the ER’s lifeblood: they triage, do assessments and exams, assist with dressing changes, coordinate with labs for tests, help patients get home when they’re discharged and much more.
Our nurses had been voicing their concerns about overcrowding and other issues for years with hospital administration and the province, and were often dismissed out of hand. So it wasn’t surprising when, in the first six months of the pandemic, they began leaving for other jobs in health care, like working as a nurse in light industry or at a family clinic—jobs where they don’t work weekends and nights, where they aren’t faced with abuse and threats, where they aren’t in a constant state of burnout. We dropped from 15 nurses to seven, then to five. A couple left on maternity leave, but most left for other, less taxing health care jobs. I can’t blame them. The ones who remained were deeply demoralized.
They also felt terribly betrayed during COVID. For more than a year, they had come to work, putting themselves in just about the highest-risk place you could find yourself during a viral pandemic. They saw what had happened in New York City and in Italy: doctors and nurses dying, patients’ beds overflowing into parking garages. They stayed anyway. When vaccines finally became available, the province’s chaotic, disorganized rollout meant that front-line workers weren’t necessarily the first to get them. We often saw people doing virtual medicine, and other low-risk professionals, getting shots ahead of ER staff.
This May, for National Nursing Week, our hospital administration gave each nurse a cookie as a thank-you. All I could think was: These people have been running around in gowns and gloves and masks and shields for two and a half years. And you give them a fucking cookie?
***
Once our ER dropped to five nurses in June of 2022, I knew that was it—it’s impossible to run a department with such a small staff. Our nurses were already working a shift, going home, having supper and playing with their kid or dog before coming right back. It was unsustainable. We were doomed. The hospital administration met on a Friday at the end of June to discuss the possibility of short-term closures. One idea was to close overnight through the summer. By Monday, this had leaked to the press. The emergency staff were stunned. Administration simply expected us to accept the idea.
Then, within days, we lost two more nurses to COVID absences. Suddenly we were at three, a perfect scapegoat for a full ER closure. One staffer reached out to our malpractice association to ask about the repercussions and risks to community members, and to our patients in ICU and the rehab ward, if we closed. What if someone had an embolism after an orthopedic surgery and all the ER doctors were at home on the couch?
The administration agreed to keep one ER doctor in the hospital 24/7, in case someone came in with a real emergency or an issue that was quick and easy to treat, or in case something happened on one of the floors. It felt like a tiny win.
Beginning on July 2, the ER shut down, a closure that stretched from one week to two to most of the month, until July 24. Those were quiet shifts for me. I treated one guy who came in with an allergic reaction to bee stings. I watched the maintenance crew polish the floors and patch up the walls. I literally watched paint dry. I continued working in my family practice nearby while the ER was closed, and one day, a woman came in alarmingly short of breath. Normally, help would have been 100 metres away in the ER. Her situation was potentially life-threatening, and I had to send her 20 kilometres down the road, to Smiths Falls. She survived, but it could have been much worse.
The nurses who quit didn't disappear into some cosmic black hole. But we're going to have to work very hard to regain their trust.
Politicians still insist the ER crisis is not so dire. In August, Ontario Premier Doug Ford said, “Ontarians continue to have access to the care they need, when they need it.” This was days after approximately two dozen Ontario hospitals reduced service over a long weekend. In Nova Scotia that same month, Premier Tim Houston said, “If you get sick in this province, you will get extremely good care. Shame on anyone who suggests otherwise.” In July, the Nova Scotia NDP obtained freedom-of-
information data showing that 43,000 people left that province’s ERs in 2021 without receiving treatment, presumably due to interminable wait times.
Across the country, more closures are piling up, too many to count. In British Columbia, the Dr. Helmcken Memorial Hospital in the town of Clearwater—one of the only hospitals in a vast rural area—has been closed more than 60 times this year. In Alberta, small-town ERs have been closed, or left with only nurses, dozens of times. Ontario has had more than 80 ER closures so far in 2022, including the shuttering of the ER in the little town of Chesley, which closed in early October due to a shortage of nurses. It’s not scheduled to reopen until the beginning of December. This fall, a leaked report on ER statistics obtained by the province’s opposition Liberals showed that on any given day in 2022, the average number of patients waiting in emergency departments for an inpatient bed was 884—a 53 per cent increase over 2021.
People’s lives are hanging in the balance here. At Great War Memorial, we’ll never know exactly what patients or problems would have come through our doors if we hadn’t been closed. We’ve since hired a few new nurses, but we’re still relying on agency nurses—temporary workers provided by private staffing agencies. As good as they are, they’re not a lasting solution. The provinces love to talk about tight budgets and yet, across the country, they’re paying agency nurses double what their union counterparts make.
Even with better pay, nurses aren’t going to come back unless there’s a firm commitment to mitigating violence and burnout and improving patient safety. The nurses who left Great War Memorial haven’t been raptured; they didn’t disappear into some cosmic black hole. They’re out there, and they’re addicted to emergency medicine, same as me. But we’re going to have to work very, very hard to regain their trust.
***

I’ve seen firsthand what it looks like when structural failures strip medicine of its patience, compassion and humanity. In 2010, one of my three children, Hilary, found a lump in her breast. I told her it was probably a cyst, nothing to worry about. I was wrong. Weeks before she graduated from university, she was diagnosed with stage-four metastatic cancer.
I knew Hilary was going to die, but I wanted her to have as full a life as possible. When she was diagnosed, her oncologist in Kingston said, “Don’t treat her, she’ll be dead in six months.” I was so incredibly angry. We found another oncologist, who was very kind, and we got more time together. For six years, Hilary was in and out of hospitals and doctors’ offices, and so was I, beside her. There was chemotherapy, radiation, multiple surgeries. We encountered wonderful doctors and awful ones.
Through my daughter’s experience, I saw medicine from a different angle, and I was shocked. After meeting some of her doctors, I thought, Why are you even here? You’re in the wrong profession. But now I think that maybe they weren’t simply bad doctors—maybe they too were burned out, at the end of their rope, having given all they could. Either way, they shouldn’t be looking after vulnerable people. My wife and I came away wondering what it must be like for patients who don’t know how to advocate for themselves or their families. Our daughter, had she been on her own, would have been lost.
Hilary’s illness and death in 2016 had a profound impact on the way I treat people. I’ve recommitted myself to being as caring as I can. No matter the day, I try to make every patient encounter meaningful. It’s not just “Here’s the literature, here are your pills, get out.” It’s “How are your kids, your cows, the family dog?” I try to get patients to see me as a navigator through a health system that is extremely complex and often unfriendly. Ideally, I’d give people as much attention as they need, but there is so rarely the time to be as decent as we should be.
I am only one person, one doctor, in one town. We need a systemic transformation to restore a health system in which doctors and nurses have enough time, energy and empathy, where people aren’t learning of terminal illnesses in the ER, where desperately ill people are not warehoused in hallways.
Governments across the country are putting on a brave face. But there needs to be real talk among the premiers and the federal minister of health, Jean-Yves Duclos, about what is going wrong. I’m hoping for a national study, a forensic audit—efforts with teeth. If you’re going to avoid crowding in emergency departments, you need to avoid crowded hospitals. That means more funding and more beds. It means improved access to home care and long-term care, so patients have places to go besides the ER and don’t spend three months in the hospital after fracturing their hip.
After decades in emergency medicine, I’m still passionate about what I do. At our hospital, we have a great foundation to build on: community support, committed physicians and nurses, and hopefully, leaders who recognize the jewel that they have. If we get through this winter and further COVID waves intact, we can become whole again. The people I’ve met over the decades in emergency represent the very best of what medicine is, and they try extraordinarily hard to make a flawed system work. That’s why the best of us do what we do, and why it’s been so painful to see some of the best of us leave.
This article appears in print in the December 2022 issue of Maclean’s magazine. Buy the issue for $8.99 or better yet, subscribe to the monthly print magazine for just $39.99.